When your wife has stage 4 metastatic breast cancer, and has been hospitalized once for an upper extremity DVT, once for pneumonia, another time for malignant pleural and pericardial effusions, has had small pulmonary emboli, and then gets diagnosed with leptomenigeal carcinomatosis, and you also live in a world that has Google, so you can type in those terms (or worse click on the links some idiot put in a blog post) and get very detailed descriptions of these diagnoses and, more importantly, their prognoses, then, despite the doctors not coming right out and telling you so, you kinda have to face it that the most likely hand you’ll get dealt this year is to watch her die. Not just the mostly likely hand, but the most likely 99 hands.
We’ve tried from the start (of the stage 4 diagnosis), before the more in-your-face evidence (which for me was the hospitalizations) not to live in denial, and not to keep things from our two teenagers or our family or community. To make decisions taking this possibility/probability into real account. But this turns out to be much more difficult that I expected.
 So this post is about a concept called Death Straight Talk (let’s call it DST. That way it sounds like the more familiar “DNR”). There are three arenas in which I want to talk about DST: 1) the medical world, doctors, nurses, and Medicine as an institution; 2) family, friends and community; and 3) the metaphysics of probability and how we think about our future. So here we go.
So this post is about a concept called Death Straight Talk (let’s call it DST. That way it sounds like the more familiar “DNR”). There are three arenas in which I want to talk about DST: 1) the medical world, doctors, nurses, and Medicine as an institution; 2) family, friends and community; and 3) the metaphysics of probability and how we think about our future. So here we go.
1) DST in Medicine: Hospice operates on an agreed-upon basis of DST. The idea is that “there’s nothing left to do” to prolong life (meaningfully), so shift the medical care to comfort, pain control, and getting the most of out each day. A Do Not Resuscitate (DNR) order is another form of DST in medicine, where the patient gets to issue a token that goes in their chart saying something like, “Look, I’ve thought this through and I’ve come to the conclusion that death is preferable to life after resuscitation, so let me go.” These are both DST items that have been embodied in institutional practice, the first at a more macro level, because, it turns out, Hospice care ties in deeply to the structure of how and what things get paid for and who gets to decide. (This in itself is worth a whole other post, but life’s too short for me to dig into that.) The second is at the more micro level, because it’s just about what to do under certain circumstances for an individual patient, whether in hospice or not.
These two patterns, Hospice and DNR, are formal recognition that near death, things are different, and we have to act differently. But now to my direct experience: despite an ominous prognosis, Ellen’s not at either of those two points yet, and so, institutionally, there’s practically no DST. It’s like a binary switch: either we act like you won’t die, and plan our doctoring on that, or we finally give up and off you go to Hospice. Here’s how this plays out. Hospitals are places full of protocols: vitals every 2 or 4 hours, neurological checks every hour, gotta pee before you get discharged, NPO (nil per os – no food or drink) before surgery, start a bag of fluids for practically anything, keep for observation for two days after X surgery, don’t go off the floor (or out of the ward doors), and on and on. Lots of protocols, mostly in place for good reasons.
But here’s the question: if you might have only 4-6 weeks left of life (if the current spread of cancer doesn’t respond to therapy) do those protocols apply? Should you really spend those two days under observation, living a substantial percentage of your remaining life in the hospital instead of at home? Should you really have that conversation you’re having with your family or friends interrupted so the nurse can write down your blood pressure numbers? Should you really have to spend the more than an hour a day (once you add it up) explaining your complex medical history over and over to each new nurse, resident, attending, etc., who comes to check up on you? Should you really get filled with IV fluids before a surgery to offset the dehydration risk that comes from the NPO protocol, which is there to mitigate the risk of throwing up under anesthesia, when those same fluids have a high risk – shown in the previous hospitalization – of causing swelling in your legs and feet which might make it painful to impossible to walk in your last weeks of life?
In our experience the protocols just don’t take into account DST. Here’s how I know: during our last hospital visit, I explicitly told nurses and doctors a story that approximately went like this: “Please treat us as if Ellen’s chart had a big DST sticker in it. It’s kind of like DNR but stands for Death Straight Talk , which, like a DNR, is treatment instructions for you from Ellen, but what it means is: first of all, we can, and do, talk about death straight, but second and more importantly, in providing your care, think about whether your actions are appropriate for someone who will likely die soon.”
The results of telling this story were clear: after some initial shocked looks, we got different care. The doctors let us go home “early” after Ellen’s Ommaya reservoir implant; we got “off-floor-privileges” while awaiting surgery; they didn’t make Ellen start on fluids at midnight before the surgery, etc. The humans involved responded deeply and with compassion to the truth that was embodied in a simple acronym: DST.
2) DST with family, friends, and community: If you want to create drama, lie. Lie explicitly, unconsciously, or by omission. In our case, we might call that Death Curvy Talk, or Death Denial Talk (DDT). The other night Ellen and I watched a dumb movie called “Meet My Valentine,” which is about a guy diagnosed with terminal brain cancer who decides not to tell his family but instead find a replacement husband/father for them instead. As a movie it was really dumb because that DDT was so obviously poisonous. But as a metaphor it’s revealing. If I look at where things feel twisty and drama-filled and out of whack, I see that I haven’t lived up to DST. As I said at the beginning of this post, we’ve tried to face things directly from the start. But something interesting has happened since the introduction of the DST acronym. As a token that we can refer to, it’s given us permission, or an opening, or something to actually get to to the straight talk more quickly. Now that it’s there, we invoke it. “Hey, I have a DST thing…”
Here’s a quote from an e-mail from a friend: “I wanted to offer to help, if need be, to begin/continue/whatever, discussion of burial, funeral directors etc. I have, unfortunately, intimate experience with this recently, as you know, and might be able to bring some perspective to this part of DST.” What a relief and and efficiency that this provides. It feels to me that the more I live into DST, the more this experience goes from what I call “dramatic” to what feels “powerful” or “moving.”
3) DST metaphysics and probability: Here’s the problem with DST. It assumes we know the specific future. Of course in one sense we do. All of us will die, we know that, but that’s hardly a specific knowing. So, using DST, how do we also talk straight about that one other hand of cards out of the 100–the one in which it turns out that Ellen recovers and later quietly dies in her sleep at the ripe old age of 103 well after I’m gone? This is the hard part for me. I used the metaphor that Ellen’s disease prognosis is like drawing a hand of cards. But that’s, at the very best, only a partially valid metaphor. Probability provides a great tool set for assessing aggregate outcomes, but it also can have the effect of deep dis-empowerment at the individual level. Just because your chances of getting breast cancer go up by X% if you have the BRCA1 mutation doesn’t mean that you don’t have any agency in whether it actually happens in your own body. From all our reading, it’s pretty clear to us that cancer as a bodily process is connected to the immune system, which is deeply connected to the central nervous system, and also connected to physiological terrain. So what power does that mean we actually have? I believe that diet, and stress, and my thoughts have an effect on “my chances” of getting cancer, and these are things I have control over. Bookstores, however, are filled with conclusions from this that to me are just magical thinking: that you can just think yourself back to health. But I also read and hear people jump to “don’t blame the victim” as soon as you mention the ways in which we do have agency. It’s kind of a double bind: if you believe in agency, then if you got sick or don’t heal yourself it’s your fault. But if you just take it as luck of the draw (i.e., not your fault) then how can you activate where you do have agency?
So to me this is where I don’t know how to have real DST. What is the “straight talk” that both acknowledges and deepens the agency we do have, and yet doesn’t fall prey to either magical thinking or blame-the-victim? Just because the odds are 99 to 1, does that mean we have to match the relative percentages of our talking time to those odds?
I don’t know the answers to these questions. But the core move in DST gives me guidance: open myself to what exists, or at least turn towards it rather than away.
Modern disease prognoses provide odds based on existing historical records: scientific studies. Open myself to them. But also the evidence of agency affecting cancer outcomes exists. Open myself to it. My pain and my joy in these days exists. Open myself to both of them. Paradoxically, denial and hiding and self-veiling also exist. So that’s OK, too; turning-toward will also periodically involve turning-away. This isn’t about some moral claim. It’s just a wish, a longing, perhaps a stance, to turn towards what I see in front of me. DST. Last words: just because I don’t wish to turn away from that which I do see, that doesn’t preclude me from turning toward that which I don’t see: all the potential branches of the future. Because what else is creation?
–Eric Harris-Braun
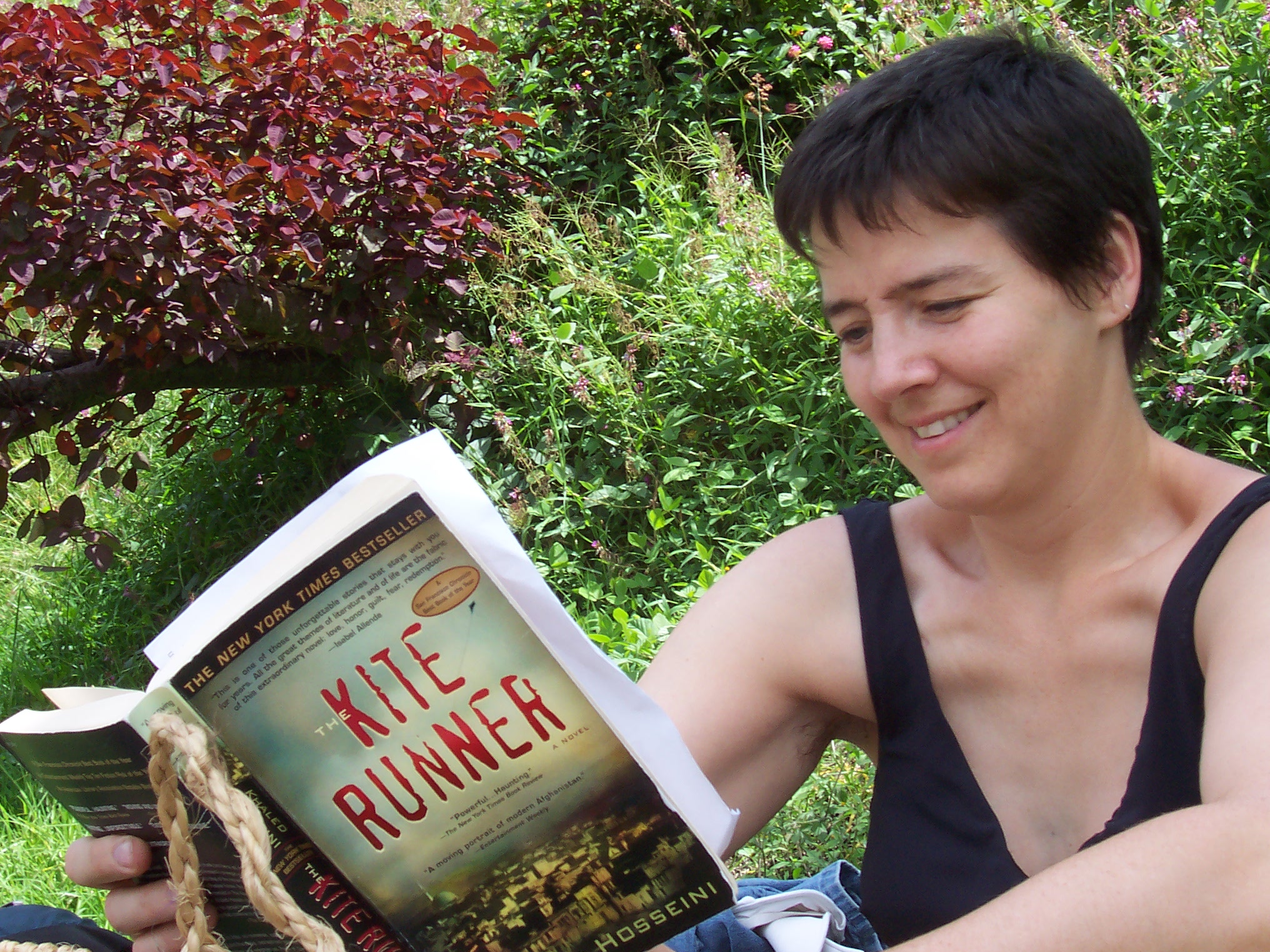 Here is one of my favorite photos of Ellen, taken one time when we were at the Cunuñacu hot springs in the valley below Quito, Ecuador. Do you have a favorite photo of Ellen you’d be willing to share with the family? If so, please send high-resolution versions by email (don’t worry about MB size) to Ellen’s sister Deb at debra@huntermorgan.com. If you can provide the date, location, and names of others in the photos, that would be helpful.
Here is one of my favorite photos of Ellen, taken one time when we were at the Cunuñacu hot springs in the valley below Quito, Ecuador. Do you have a favorite photo of Ellen you’d be willing to share with the family? If so, please send high-resolution versions by email (don’t worry about MB size) to Ellen’s sister Deb at debra@huntermorgan.com. If you can provide the date, location, and names of others in the photos, that would be helpful.






 broken?
broken? Just wrenched and swollen?
Just wrenched and swollen? don’t let the foot move!
don’t let the foot move!