This update goes on an on but trust me, I am leaving out some non-essential but confusion-increasing twists and turns.
I had my 3-month CT scan February 10th. At an appointment to discuss the results two days later, my oncologist said that the radiologist’s report said the metastasis in my lung had grown a bit (one dimension had been holding steady at 1.4 cm and is now 1.9 cm), which meant it was becoming resistant to the chemotherapy. We discussed options. I had a “we knew this day would come” sinking feeling. Is it all going to be harder and more confusing from here onward? Besides waiting for a more clear signal of growth, or switching chemotherapy, the other option was to use stereotactic radiosurgery on the lung met. If the rest of me was still responding well to the Eribulin, but this lung met had developed resistance, we could kill it off and I could go on my merry way with Eribulin for longer. That seemed like a bearable plan.
But he called me later in the day to say the latest version of the CT report–not the preliminary report he had had in the morning–actually said the lung met was stable. Whaa? Later he reviewed the images himself with a radiologist and told me “you could go either way” because something is measuring bigger, but is it tumor or is it associated collapsed lung tissue? No one can quite tell. So that was nice news. But we stuck with our plan to have me talk to the radiation oncologist (the brain-zapper) because if the lung met had grown, we could zap it. The idea of getting that lung met off the list definitely had some appeal.
Then on Friday the 13th (oh yay) I had a follow-up brain MRI to check results of the January zapping. (“What? I am having a brain MRI to check for brain tumors and you want me to have it on Friday the THIRTEENTH?”) But I did.
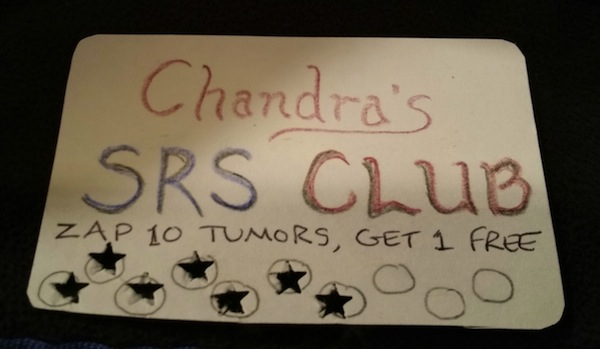
On the 18th we met with the radiation oncologist. The MRI showed good response to the zapping of two mets (yay) but one tiny little worrisome dot in the brainstem is still there. We wanted it to disappear, which it didn’t. But at least it’s not any bigger. Good news, bad news, good news. Next, more bad news: he spotted another little tiny stable dot somewhere else. “This is most likely a tumor also,” he said nonchalantly. Great. Hey buddy, this is your something-thousandth brain met so it’s all in a day’s work to you, but to me, hey, this is only my…counts on fingers…8th or 9th! So show some respect. (Dot #2 was on the November MRI but wasn’t noted then, and it wasn’t on earlier MRIs. So yeah, most likely a tumor, but again–good news–not any bigger for 3 months).
But the real kicker was when he reviewed the CT scan with us. I like this guy because he calls up all the images on the computer and lets us look, and fiddles with them and compares them, and we get to see how he does it. It’s kind of mind-blowing to realize that though they use high-tech machinery and chemicals and stuff and measure things by clicking with the mouse, in the end, they are just LOOKING AT PICTURES and deciding whether deadly growths have grown or not.
So anyway, he calls up the February CT scan and the November CT scan and we compare them. He does some measuring and doesn’t come to any conclusions that way, but we all agree that the met looks “fuller” or “more plump” or “filling in” compared to how it looked in November, despite maybe measuring almost the same in its extent. This met is like a little raisin with a couple of tentacles, and the tentacles are the collapsed lung tissue (or atelectasis). So the open question is: is the fullness caused by tumor cells growing out from the main tumor along the tentacles, or is it just more collapsed lung developing at the margin of the tumor? The zapper is not sure, but thinks it is probably tumor growth. Which means we should zap it, because that means the Eribulin is not working on that tumor anymore. If we zap it successfully, then I can stay on Eribulin because it is working everywhere else it is expected to work (meaning, not in the brain but in the body).
But that’s not the kicker. Because next he says, contemplating the scans on the computer, “If I were betting, though, I would bet that this is a primary lung cancer, not a breast-cancer met. It looks like one. Breast-cancer mets in the lungs are not made of lung tissue–they’re a foreign type of tissue, so they grow in a ball and push the lung tissue outward. Not in a blob with tentacles like this.” (Well maybe he didn’t say “blob with tentacles” but that’s what he meant.) “Have you ever smoked?”
WHAT????? So I tell him a) I have never smoked a single cigarette, and b) what are the chances that I would be discovered to have stage IV breast cancer and primary lung cancer at the same time? Come on, now. He agrees that it seems unlikely given the circumstances, but still….it sure does look like a stage I lung cancer to him.
“Stage one!” I say. “That’s the first good thing you’ve said all day.”
We determine that yes, I had the sternum met biopsied and that one was definitely breast cancer. And no, I didn’t have the lung met biopsied. So do I want to biopsy it now? Because if it’s lung cancer the standard of care is to do surgery, remove the upper lobe of the lung where the tumor is located, and take out the lymph nodes nearby. “What about this situation is standard?” I ask incredulously. He takes my point. He says that though lung surgeons would certainly want to operate, surgery might rev up the metastasis in my body and that would be bad. So he would suggest zapping it instead, the way they do when someone with lung cancer is too frail to withstand surgery. The “control rate” is not proven to be quite as good as surgery, but the side effects are less frequent and less severe.
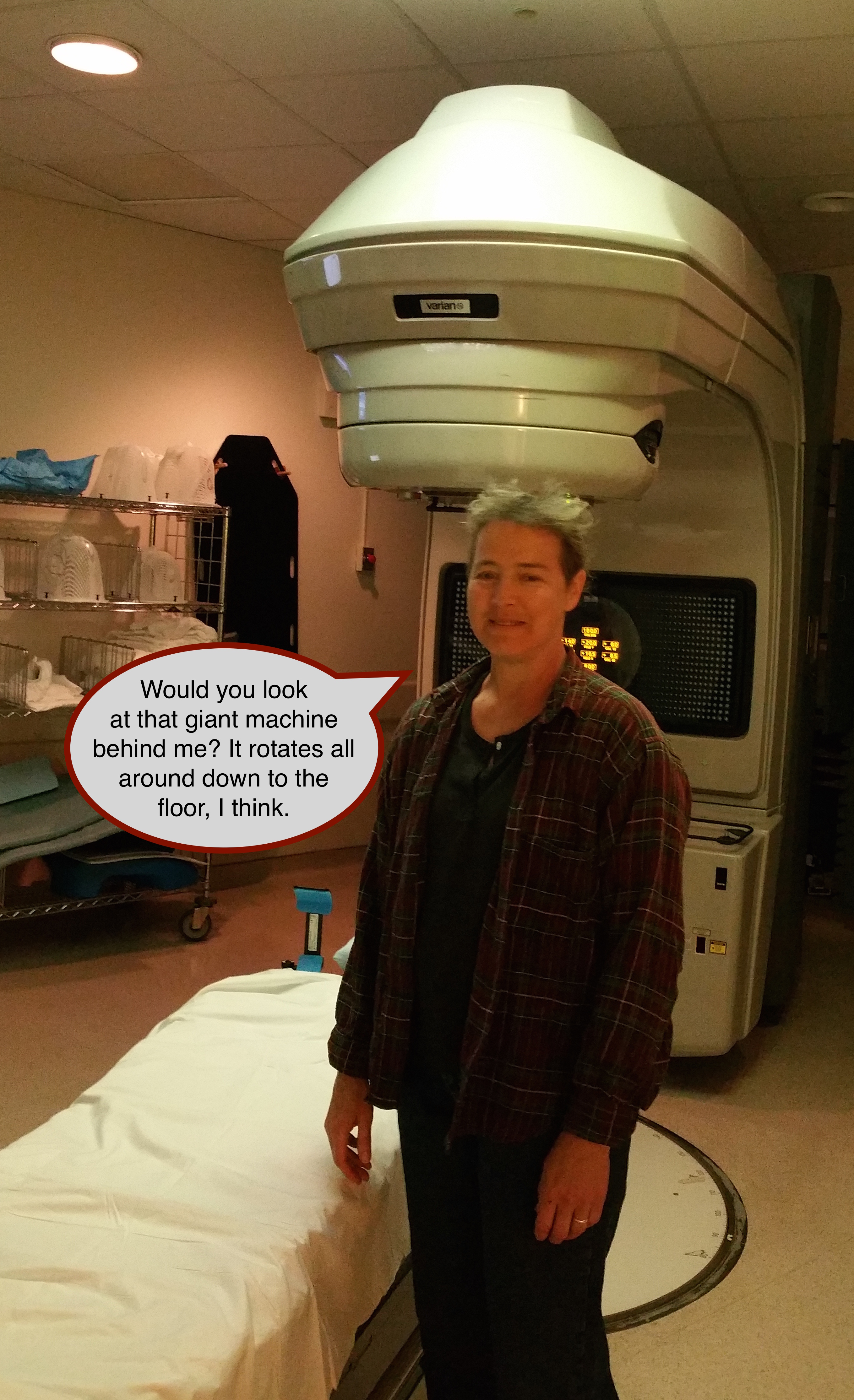
The zapping is a bit more complicated than the brain zapping–five treatments over two and a half weeks, and they have to restrict my breathing some so the lung doesn’t move during treatment, and there is a risk of rib damage from the edge of the radiation field. But basically, a low risk of side effects, and I still have a whole right lung (which I dunno, I feel I need to keep if possible). Besides, if he only gets to zap frail people, I probably am less at risk of side effects than them, right? Being not frail.
“So,” I sum up after a while, “whichever it is, we would zap it. So therefore why would I biopsy it? A biopsy doesn’t give me information that changes how I would proceed.”
Though he sheepishly says, “Just to know?” he agrees that there is not a strong case for biopsy. He says he’ll review the CT scans with a chest radiologist and argue with the lung surgeons over me. “They’ll be mad at me,” he says. I say this situation would make a great Grand Rounds presentation about uncertainty and patient choice so he must invite me when he presents it.
Whew. What a roller-coaster. We leave and I begin trying to figure out how lung-zapping is going to fit into my chemo schedule and my non-cancer-related life in the next month or so.
Then the next day my oncologist calls, having gotten the latest update from the radiation oncologist. The consulting chest radiologist (whom the oncologist thinks highly of) also says it looks like a primary lung cancer, but says he doesn’t think it’s actually growing. And when I inquire, my oncologist says sure, he’s seen breast mets look like this before. He agrees that the lung-cancer hypothesis is a little hard to swallow given the circumstances. So, given all the opinions, he comes down strongly in favor of this plan: no biopsy, for goodness’ sakes no lung surgery, and right now no zapping, either–just wait and see what the next CT scan says in three months.
And that’s where we are. At least until the next phone call.
 Glimpse of oncologist using his wiles to get me moved to the oncology area, a better neighborhood of the hospital
Glimpse of oncologist using his wiles to get me moved to the oncology area, a better neighborhood of the hospital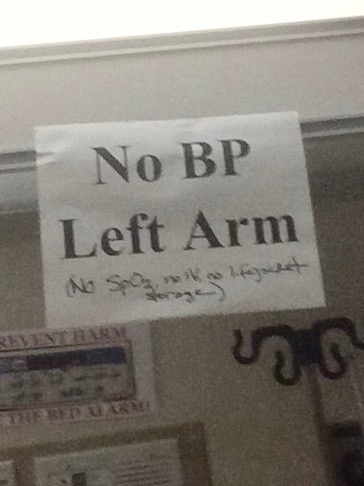 Had to add a few more equally obvious Don’ts.
Had to add a few more equally obvious Don’ts.