Obituary
Ellen Key Harris-Braun, 50, of East Chatham, New York, died at home Friday, October 28, 2016. Born in Atlanta, Georgia, she attended high school in Rochester, New York, and graduated summa cum laude from Yale University with a BA in anthropology. A life-long science fiction reader, she turned her honors thesis on the use of anthropological concepts in science fiction into an application to Del Rey Books, the sci-fi division of Random House. There, in the early 90s (before the Web) she began an email newsletter, including writing advice, that ultimately became the independent Online Writing Workshop, which she and her husband, Eric Eugene Harris-Braun, directed. During her last few years at Random House, she was part of a pioneer group in charge of that publisher’s online projects.
Ellen was a midwife. She trained as a childbirth instructor after the birth of William, her first child, then became a doula after the birth of Jesse, her second. As she began her midwifery studies, she served first as a public member of the Commission for the Accreditation of Birth Centers and then as director of data development for the Midwives Alliance of North America’s division of research. As a Certified Professional Midwife, she attended home births in Massachusetts and New York, working with River and Mountain Midwives and Local Care Midwifery.
She and Eric designed the data collection software for MANA’s statistics website, an ongoing project that recently led to the publication of a landmark study of almost 17,000 planned home births. In 2014 she received the MANA Star Award for her contributions to the profession, and that organization has named its two research awards (one for students, one for practicing midwives) in her honor. In 2015 the Midwifery Institute of Philadelphia, where she had been pursuing graduate studies, established the Ellen Harris-Braun Midwife Scholar Award and presented the first one to Ellen.
Her love of words and her sharp wit – often described as not TSA-approved – were relished by her friends and family and have been passed on to her children. Evidence can be found on her blog, World of the Sick/World of the Well, an account of her illness that is at once informative and, almost to the end, a delight to read (ellen.harris-braun.com).
In addition to her husband and children, Ellen is survived by her mother Kathryn Key Montgomery of New Orleans; her siblings, Anne Montgomery Hunter of San Francisco, Debra S. Hunter of San Rafael, California, Lisa M. Hunter of Madison, Wisconsin, James Paul Hunter of Atlanta, and their father James Paul Hunter of Charlottesville, Virginia; her step-mother, Laurie Randolph Barili Harris of Atlanta; her brother- and sister-in-law Jens and Spee Braun; ten Harris cousins; and beloved members of the Quaker Intentional Village-Canaan. Her father, David Jesse Harris of Atlanta, preceded her in death.
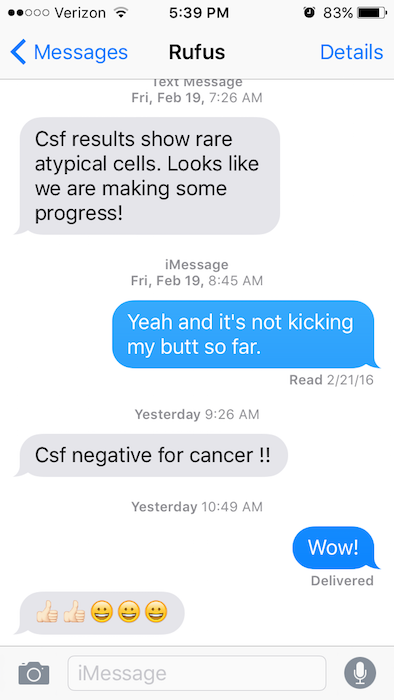
A memorial service will be held at 11 am Saturday, November 12, at the Old Chatham Quaker Meeting House. Her family and friends are grateful to the helping circles that have sustained them and to Rufus Collea, MD, Elizabeth Hanlon, RN, and Jeffrey Arp-Sandel, MD. Memorial gifts may be made to the Ellen Key Harris-Braun Research Fund at the Foundation for the Advancement of Midwifery (www.foundationformidwifery.org).




 One gorgeous October day after the next comes and goes, and the moon now wanes after filling the eastern sky with magnificent moon rises these past evenings. Ellen has endured increased pain and discomfort, and her caregivers adjust this and that to find the best way to ease her journey. We wonder how much longer she can persevere and whether we have done an adequate job in helping her complete what she needed to get done and in giving her permission to let go and die.
One gorgeous October day after the next comes and goes, and the moon now wanes after filling the eastern sky with magnificent moon rises these past evenings. Ellen has endured increased pain and discomfort, and her caregivers adjust this and that to find the best way to ease her journey. We wonder how much longer she can persevere and whether we have done an adequate job in helping her complete what she needed to get done and in giving her permission to let go and die.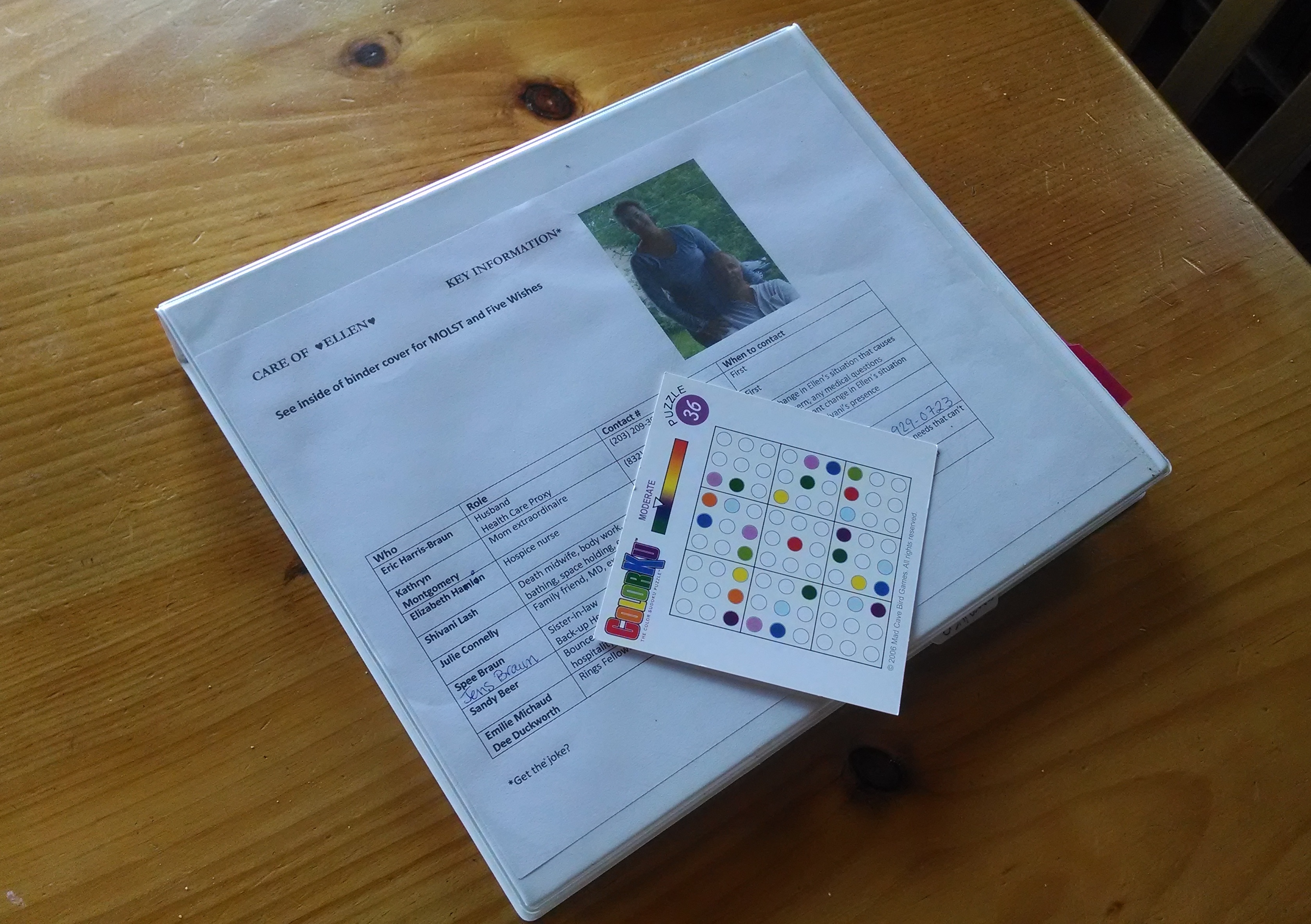 Clipboard - The clipboard goes back and forth but mostly can be found on the bedside table upstairs near Ellen. It holds a chart on which the person at her side can track her sleeping and check timing of medications and comfort measures to ensure they are administered relatively close to “on schedule” - sometimes a challenge, as we don’t want to wake her to give her meds.
Clipboard - The clipboard goes back and forth but mostly can be found on the bedside table upstairs near Ellen. It holds a chart on which the person at her side can track her sleeping and check timing of medications and comfort measures to ensure they are administered relatively close to “on schedule” - sometimes a challenge, as we don’t want to wake her to give her meds.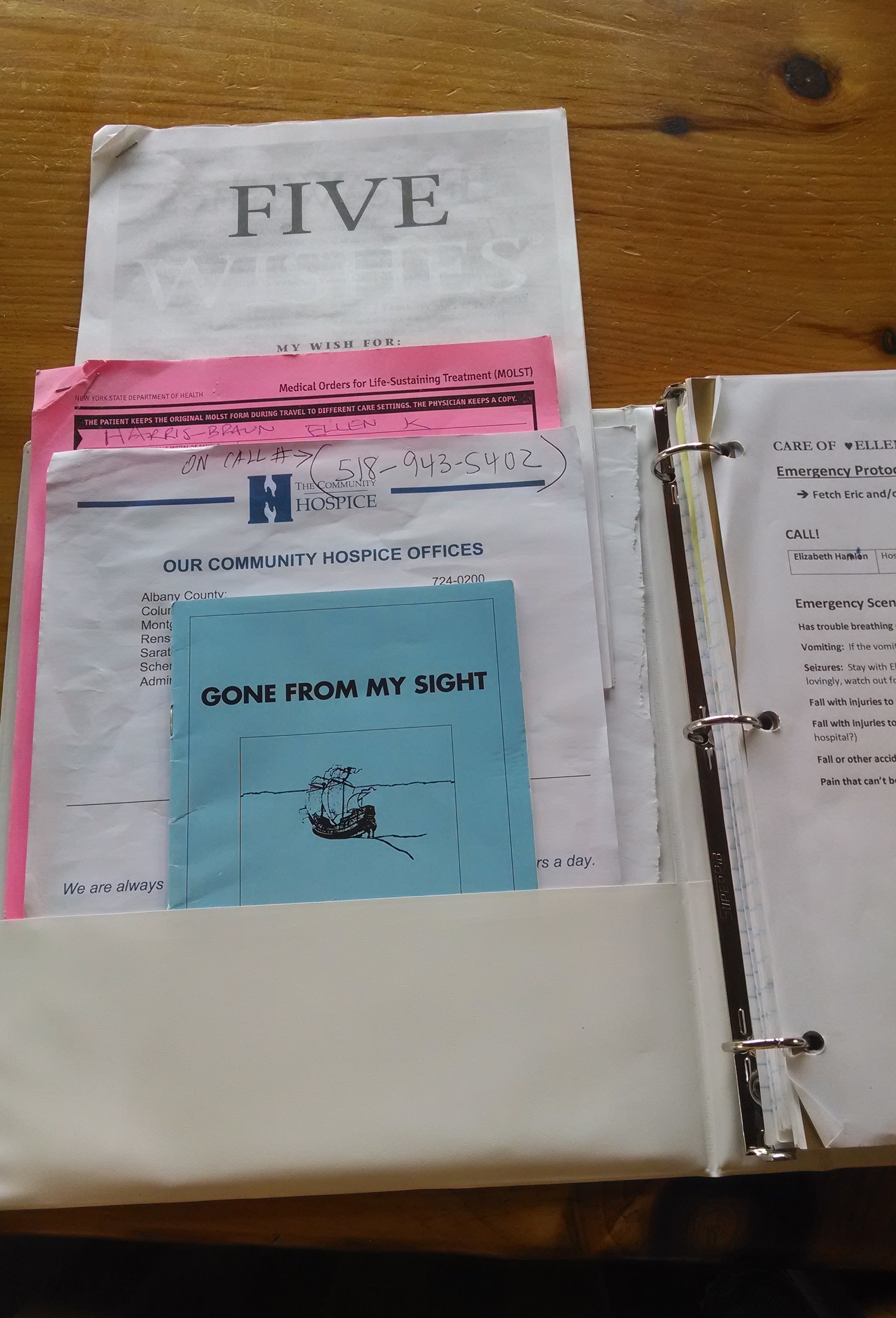 log that might be of use to other caregivers. It turns out the log serves other purposes, one of which is to help an individual caregiver decompress after time with Ellen, even dump out one’s thoughts and feelings in a cathartic way.
log that might be of use to other caregivers. It turns out the log serves other purposes, one of which is to help an individual caregiver decompress after time with Ellen, even dump out one’s thoughts and feelings in a cathartic way.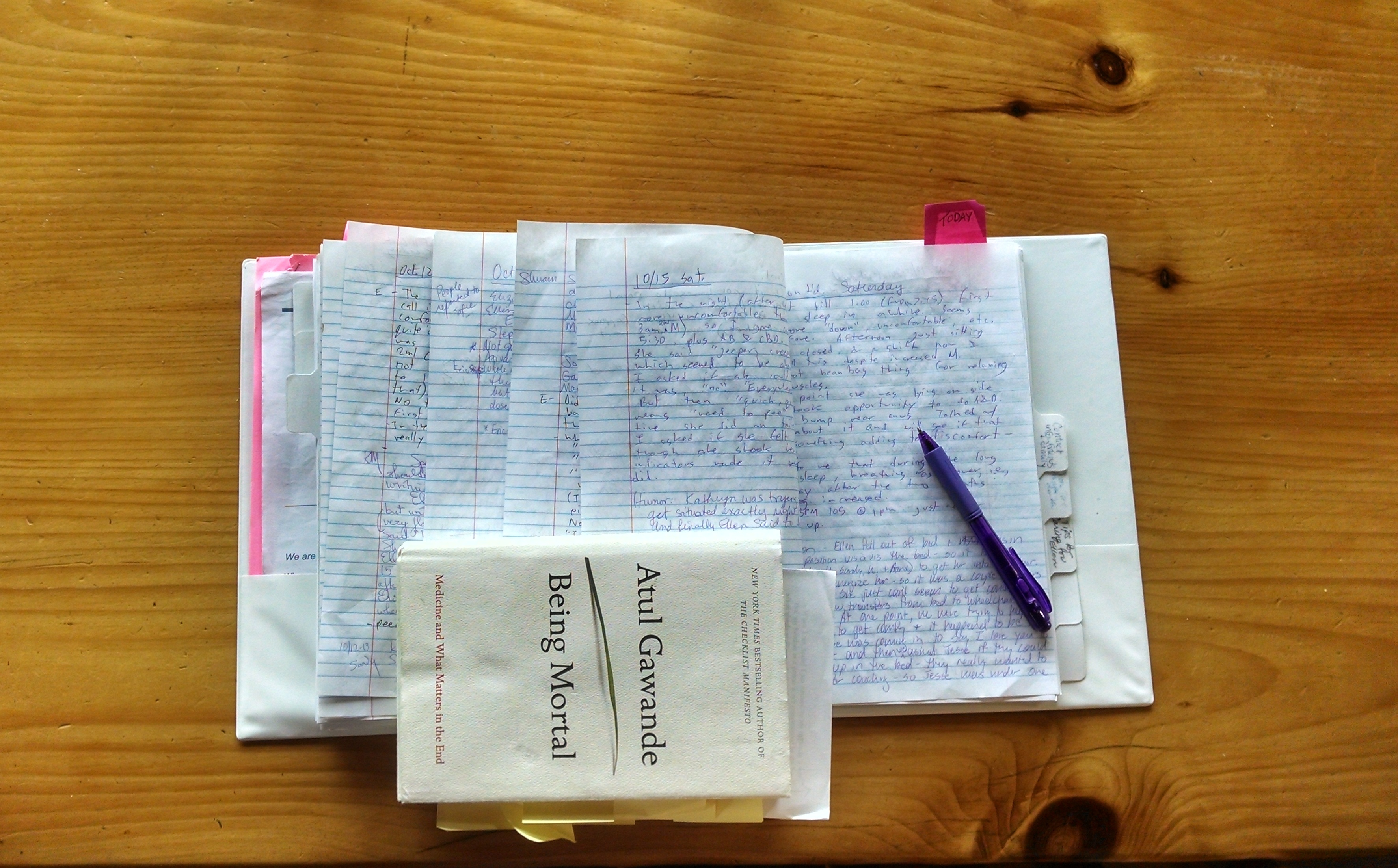





 Nut butter mementoes left by our helpful visitors!
Nut butter mementoes left by our helpful visitors! Charging my apple
Charging my apple