Two years?
Yesterday was the two-year anniversary of when I found out I had stage IV cancer.
Yesterday was the two-year anniversary of when I found out I had stage IV cancer.
It’s Sunday afternoon and guess what? I still have pneumonia. (I have to keep reminding myself of this to explain why I am still so, so, so very tired and worn out.) We came home late Thursday afternoon and I keep waiting to notice I’m feeling better, but I don’t notice. I am doing much less coughing, though.
I didn’t have a headache at all on Wednesday or Thursday in the hospital, but we can’t figure out why. Oxygen? Antibiotics? Now that I’m home the headache is back, which is really getting me down.
Anyway, the plan for the next week is: rest as much as possible, take antibiotics, and eventually feel better. Then the week after that, back to chemo. I guess I’m just skipping the second dose of round 29.
I got good news today at my oncologist's office—my brain MRI yesterday turned up no new spots of cancer (in 4 months—my last MRI was June) and the ones zapped in May continue to cooperatively die and fade away. So that is really great. I don’t need more of that right now. Too much else to deal with!
My left arm, upstream from the original blood clot in my brachiocephalic vein, has now developed some lymphedema so I have to go deal with that at the lymphedema clinic—not that it will ever go away. Just more appointments and treatments and self-care regimens to incorporate into my days. Hoping it won’t get any worse.
Also, the lung CT I had on the 12th to confirm the blood clots in my lungs also showed that my “lung spots” seen on the 9/11 chest CT are “grossly stable," meaning that they basically didn't change/grow in that intervening month. That doesn’t mean that they aren’t new metastatic lesions, but at least if they are—which they probably are because they’re still there—they are slow-growing and still tiny. Or the chemo is keeping them in check right now, even though they showed up despite chemo. (That would hint that they are resistant to this chemo.)
And I got two hugs from my oncologist. He called me “sweetheart” and I let him. :) He has such energy and is so willing to meet me where I'm at that seeing him (which I do every 3 weeks, at the start of a new chemo cycle) is always a positive part of the day, even when the news is not good. I am lucky to have him on my team. I am very picky about my doctors and how they relate to me (and Eric): how willing they are to answer my many questions, how comfortable they are answering them in pretty science-y detail, how much choice they give me vs. how much direction. Whether they look us in the eye. Whether they laugh at my jokes. And how I feel after spending time with them in an exam room. I have known my oncologist since 2006, when my breast surgeon said, "You will definitely like him" and was oh so right. He is my age, within a year or so, and has a quick mind and a good sense of humor. Such luck!
We reduced my chemo dose too, because of my increasingly numb/painful left foot. It is weird that I have such serious neuropathy in one foot only--usually chemo-induced neuropathy is more symmetrical. But it is what it is--I just feel lucky that it's only one foot.
Sometimes I wonder where my time goes. Why am I not doing more "work"? And then as I apply the TENS unit to my numb foot, negotiate with the insurance company about covering my pain cream for another month, make a lymphedema clinic appointment, and remember that I had chemo this morning before that trip to shop at the food co-op and the nap, I kinda vaguely see the problem...
We always figured a trial (of a PARP inhibitor) would be my next step after Eribulin but with the headache & steroids I am probably not eligible for many trials--usually steroid use indicates uncontrolled brain stuff and researchers don't want those patients in their trials. I am tapering off the steroids but it will be a long process, if it works at all in the end. So that's disappointing, if it turns out to be the case. I am going to try to find out more about trials that are about breast-cancer brain-met treatment itself--I could probably get into those. I have a brain MRI tomorrow (the last one 4 months ago showed nothing concerning, but that is a long time to hope for a weedless garden). Then I have a consultation appointment on November 2 at Dana-Farber with a breast-cancer oncologist who has done a bunch of brain-met research (Nancy Lin).
I am feeling a bit better as of Friday–a bit more energy, a bit less out of breath. I almost felt like I could try to take a short slow walk. But this is going to be a slow recovery. Today I’ll try to start up with Qi Gong again and just take it easy on the deep-breathing parts that will be hard. And yay, my mom is coming today to help out for a few days.
England was lovely! Here's more about the trip if you're interested. I've been back a few weeks now and they have been less energetic than my time in England, for sure. I did a decent amount of walking on the trip (along with a LOT of riding the wonderful Tube) but in the last week or so my left foot has gotten more numb and more hurty and it's hard to walk very far, especially with my left knee also continuing to hurt some about half the time.
To continue with the complaints, my headache is worse in the morning and then most days goes mostly away; some days it sticks around. I recently started taking Cymbalta for general pain (it's an antidepressant but also used to treat, for example, fibromyalgia or chronic back pain) but I'm not sure if it's doing anything yet. I hope it will. May have to increase the dose. I have started going to a pain-management practice. They prescribed a compounded pain cream that has various things in it including neurontin. Not sure if that works or not yet--just picked it up yesterday after lots of insurance hassles over it (mostly handled by Eric).
Voice update: My vocal-cord damage is slowly getting a bit better, which is nice, thanks to vocal-cord therapy and tincture of time. Sometimes my voice sounds almost normal. Sometimes, especially at the end of a talky day, it is all hoarse and breathy and can't get loud. Shortness of breath, which started at the same time as the voice problems, is only a bit better. But I had lung-function tests yesterday which showed reasonably normal lung function in terms of lung volume, etc. So the shortness of breath is not that my lungs aren't working ok. I guess it's more that I'm not quite using them well enough (my diaphragm isn't doing what it should be?). However, even a bit better is noticeable.
I had chemo yesterday and last week--we're continuing with the Eribulin, giving it the benefit of the doubt, until I get my lungs scanned at the beginning of November to see what those "spots" are up to. By then I'll also have had my next brain MRI (October 26) so we'll know if anything is going on in there too.
And that's the end of the health update I guess!
I had m periodic CT scans last Friday and a bone scan too, warranted by my back muscle spasms I guess, and we meet with my oncologist tomorrow afternoon to find out the results. The Sunday after that I go to England for 8 days. That’s not very long to make a new plan if the chemo has stopped working.
Meanwhile I had vocal therapy today to work on my partially-paralyzed left vocal cord. I’m getting better, slowly. Tomorrow, an ENT follow-up appointment before the oncologist, and if all goes well, chemo too.
Trying to deal with various pains and aches these last few months, I have accumulated a wide variety of what I think of, in more humorous moments, as “cancer-lifestyle accessories”–all kinds of things people give you or you acquire because maybe they will soothe an ache or prevent a pain or cushion your knee or keep a headache at bay. Or keep you from coughing at night, or help your numb foot, or cover your head, or…the list goes on and the stuff keeps accumulating. Some of it works out and becomes (temporarily?) critical to day-to-day life. Some things you try and they just aren’t the right thing. Some things I happily don’t need now though I have dozens: hats and scarves.
Some good stuff I depend on right now–accessories that would be sold along with me if I were Cancer-Lifestyle Barbie:
A friend of mine just wrote me: “Having cancer is a full-time job, and one with lousy hours, benefits, and working conditions, isn’t it? And you can’t quit."
Love that.
The last 10 days have been better for the headaches–I’m still wearing sunglasses and closing the windowshades most of the time, but having more edge of headache or threat of headache than actual headache. Still not great, still taking a pretty high dose of steroids, and not trying to taper down yet because I don’t think I can take any more headache than I’ve got right now. So I feel kind of stuck.
A few weeks ago my good friend Birdie sent us Atul Gawande’s latest book, **Being Mortal. **It took us a while to read it but WOW. I think everyone should read it. Especially if you fall into one of these two categories:
 Here's the *New York Times* review, which tells a bit more about the author's journey through these issues. It's a book powered more by stories than by studies--very readable, and full of insights that I found really important.
Here's the *New York Times* review, which tells a bit more about the author's journey through these issues. It's a book powered more by stories than by studies--very readable, and full of insights that I found really important.First of all, on paper I’m doing great. Cancer under control still, chemo still working, few chemo side effects. May’s brain zapping showing good results (tumor shrinkage), nothing previously treated growing bigger, nothing new popping up in there in the meantime.
But in my actual life I can’t get rid of the medium-bad headache that comes whenever I try to taper off the post-zapping steroids. Usually I’m off them in 3 weeks and it’s been over 2 months since the last zap. (And I was on a maintenance dose of steroids from the previous mid-April zap until end of May, so it’s been…3 and a half months on steroids). I keep getting down to a very low dose of steroids, then get the persistent photosensitive headaches, then if I don’t increase the steroid dose again I start to throw up and feel REALLY bad after a few days and not only have to wear sunglasses until 9:30 at night but also stay in my bedroom with the shades drawn all day and avoid screens, books with too much light shining on the pages, etc. And I don’t have any appetite.
Not fun. Maybe my latest steroid regime will work better though. Got it planned out yesterday and today was definitely a better day. I even cooked for an hour for dinner! But it seems like when it’s gotten bad, it then takes a long time to get back to an even keel where a dose that should work does work.
I think at this point since there’s no swelling in my brain (the main reason I would have a headache that goes away on steroids) I probably have this:
**glucocorticoid-withdrawal syndrome** has occurred upon withdrawal of corticosteroids but was not related to adrenal insufficiency. Patients experienced anorexia, nausea, vomiting, lethargy, headache, fever, arthralgias, myalgias and postural hypotension. Symptoms resolved when corticosteroid therapy was reinstated. *http://www.drugs.com/sfx/prednisone-side-effects.html*
Happens when people have been on steroids over a certain dose for over 2 months. I have fluctuated around that certain dose. Treatment is the same...treat the symptoms with steroids, then slowly, maybe even more slowly, taper off.
So the last 2 weeks have been a taste, for me and everybody, of me being pretty much an invalid. Too tired and short of breath to walk anywhere, too headachy to go outside until dusk without a good reason, hiding in my room and being pretty miserable the whole day long. Too headachy to tackle any work beyond little tasks and responses and paying the bills. Waking up with a headache already at 6 am. I have found that frankincense essential oil on the temples and back of the neck might help the headache a little (thank you, Marcy!) and also that slathering Biofreeze, my menthol gel that I put on my knee all the time for pain, on my jaw muscles, temples, and forehead, and my neck and shoulders sometimes too, helps the headache recede a little as well.
OK boy enough rough-week update for now! But that should explain why I haven't posted much for a while.
Here is a picture of one of my favorite birds--a barn swallow. They come to play with us and raise their babies from June to late August or early September, then they go away again. It has not been such a great summer for fireflies on the hillside below my bedroom window, but we have had lots of swallows on the Land and around our house, swooping and chasing each other and cornering the sides of our house as they go for insects too small for us to see.
 Barn Swallow
Barn Swallow
I got a surprise call from my favorite nurse in Radiation Oncology yesterday (Tuesday), leaving me a message about my Monday MRI. I thought I would have to wait untold weeks and weeks to find out about the results, since I don’t have an appointment with anyone until next week (the neurologist) or the week after (chemo Day 1). Of course I wasn’t going to patiently wait that long, not being a good “patient,” but here was Joanne leaving me a message that went like this: “Dr. Chandra looked at your MRI and it looks good. Everything is either stable or smaller. Give me a call, I want to talk to you in person.”
So that was a really nice message to get yesterday afternoon, for sure. Especially because what with the continuing headache, which is dogging me as I taper off the dexamethasone finally, I was wondering if maybe I had, unexpectedly, a new crop of 12 mets or a re-growth of the original biggest one with lots of associated swelling. But no. Nothing to explain the continuing headache, and unfortunately the headache seems worse now that I’m on the last week of the latest taper–1 mg dexamethasone per day. I think from my experimenting with splitting up the larger doses (like 4 mg per day taken as 2mg in the AM, 1 mg at 1 PM, 1 mg at 7 pm), 1 mg is effective at keeping away the headache but not at making it stop. So taking 1 mg when I wake up in the morning doesn’t seem to do anything.
But the only way to get my own adrenal glands to re-start making enough corticosteroids (? haven’t read up on this again lately) is to not ingest exogenous steroids. Thus the taper. I have been on some level of dexamethasone (Decadron, steroid) since my brain zap in mid-April. It’s time to get off them! But having a headache a lot of the time really sucks. Even if it is not a really bad headache–sometimes more of a nagging one. This morning, more of a real headache.
Anyway, off to call Joanne!
If your interest in this blog extends to our July 2015 family trip to France, you can read about it and see pictures here.
OK France was really fun. But today I am too tired to do a good post about it with beautiful pictures to make you jealous of my life, etc. We fit the 13-day trip in around my usual chemo schedule so I had chemo the day before we left, and this morning (we arrived home at 12:30 am today). After chemo I had an afternoon appointment with an ENT (ear/nose/throat) doctor to check out my various throat-related symptoms I’ve been experiencing and complaining about since mid-June–the stuff diagnosed preliminarily as GERD due to continued steroid use.
I really liked the guy, despite the fact that he stuck a camera up my nose and down my throat to take a video of my vocal cords, etc. It was fun to see the video and have him explain what he saw. Which was: left vocal cord weakness and related dysfunction of epiglottis, etc. caused by damage to a motor branch of the vagus nerve that controls that stuff. This explains my weird cough, not being able to close my throat completely (like when popping ears on an airplane), my hoarseness, my lack of voice projection/loudness, my more frequent coughing while drinking and coughing when laughing, and my shortness of breath also–even though that seems like a lot.
The treatment: speech & swallow therapy. Can’t get an appointment with the speech therapist guy the ENT works with until August 11 though (bummer). Also, it has all gotten a bit less acute, so maybe it will just continue to get better on its own some more.
The cause: unknown. Maybe chemo…chemo damages nerves. Maybe the brain-zapping…somehow indirectly (I’ve never been zapped very near this nerve). The swelling from brain-zapping?
More on France tomorrow or soon!
In the Boston airport with Eric, Will, Jesse, and Jesse’s friend Lydia, waiting for our plane to Paris. Then train to Aix-en-Provence. I have a bit more energy this week, it seems, and chemo yesterday didn’t slow me down. This should be a fun trip. Though I’m sure by the time we get to where we are staying tomorrow afternoon, I will be BEAT!
However, we are staying only ten minutes’ walk from a famous chocolatier. More later!
Last Friday’s 3-month CT scans (chest, abdomen, pelvis) showed nothing new or worrisome–stable mets, so Eribulin still working! That was really good news especially since I was wondering about the cough and shortness of breath.
Chemo was easy this week. My sister Deb is visiting and being my driver plus major household helper and cooking some, too! Wow.
The weird cough and hoarseness and shortness of breath make various professionals think I have GERD from the steroids (gastroesophogeal reflux disease) even without typical GERD symptoms (acid reflux feeling, indigestion, heartburn). So I switched to a different proton-pump inhibitor to protect me better from the steroids and we’ll see. I also have an appointment with an ENT specialist to look for nerve issues (caused by GERD?) in the area of my throat that is affected–but not until after our trip to France (July 1-13).
Today’s appointment with the neurologist was good–we liked her, she spent lots of time trying to figure out my complicated situation, she listened, and she came up with good small changes to my meds to address my post-SRS headache issue and maybe improve my knee and other pain. Most excellently, she is not convinced that my little episode on May 30 was a seizure. Maybe more like an almost-faint. We will get an EEG in the next month or so which will probably show a non-electrically-disorganized brain…then it looks like I’ll be able to drive again, probably. My next brain MRI is July 21. She thinks the trouble I’ve had recovering after this zap may just be the result of having had so many zaps…it gets harder to bounce back. She does not think I need to be on Keppra (anti-seizure med) “forever” though we’re sticking with it for now.
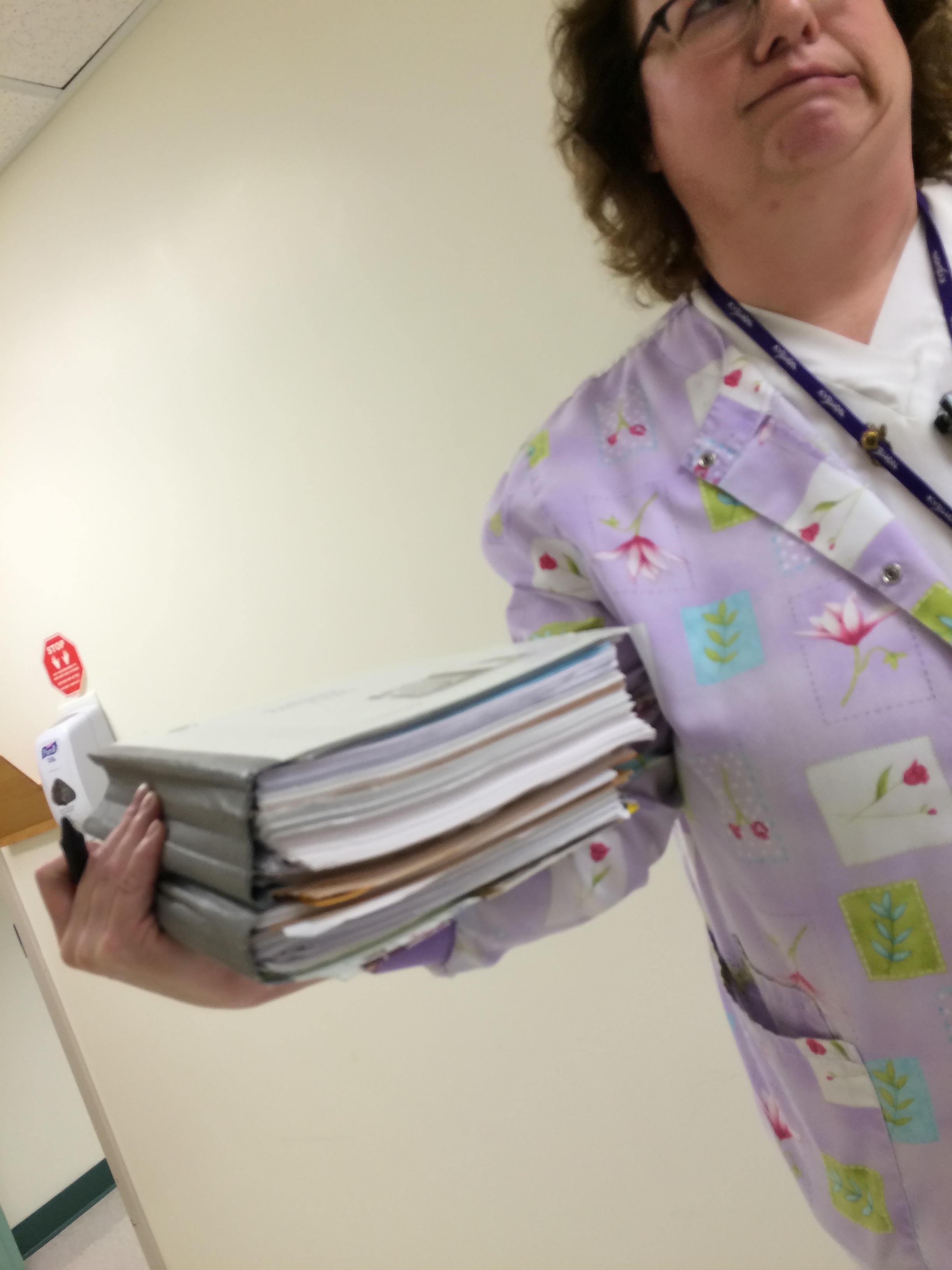 My old-fashioned paper chart at Radiation Oncology…weighing down my favorite nurse!
My old-fashioned paper chart at Radiation Oncology…weighing down my favorite nurse!
So that was the news this week. I do believe I have No Other Medical Appointments until next Tuesday’s chemo, and the day after that, all the Harris-Brauns, plus Jesse’s sweetie Lydia, are off to Aix-en-Provence for some summer living in France!
I am getting bored with how much I think about/talk about/update people about what’s going on with my annoyingly imperfectly-functioning body. It just begins to sound really dull and repetitive to me…and must eventually to others as well! I am certainly better at talking about, or just more willing to talk about, the physical goings-on than my mental or emotional or psychological goings-on, which are probably of more interest overall to others. But when I’m with other people I really don’t want my cancer life to dominate the conversation–it’s so much less interesting overall than other topics!
But it’s not just about my interactions with other people; I am getting a bit fed up with how much of my own attention my body currently requires. I wake up feeling not so good; or I can’t fall asleep because various things hurt or feel weird; I then start to investigate whether this is just tiredness from not enough sleep, post-chemo ick, post-radiation fatigue still dogging me, or did I do too much with all that going on yesterday and now I’m paying a body price? Or is something new going on that I need to pay attention to, some new symptom or side effect that needs to be reported on, treated, prevented, ameliorated? Whoof! it’s kind of tiresome. It’s another way in which cancer is taking up so much of my life–not a way I anticipated.
Argh, so frustrating to need to Rest Up explicitly in a day before tackling a task or event I want to bring even a modicum of energy to–it feels like I am an old laptop with a failing battery that has to be charged up in a pre-planned way. It’s also hard to remember that this level of fatigue is temporary (due to the SRS last week) and I will rise out of it eventually.
This morning after sleeping in, I sat on our porch surrounded by the beautiful, damp bright-green view I am lucky enough to have, of trees, grasses, wildflowers of late spring, darting swallows, sparrows, starlings…people moving around the land with more energy than I have…we drank our tea and I soaked it all in. Ahhh.
Sitting here just finishing up the first dose of cycle 23 of chemo, with awesomely normal liver enzymes, decent red-blood-cell count & white-blood-cell count, everything else all good. Now we’ll stop by the food coop and go home and I will rest some, because last week’s three afternoons of zapping gave me a lot to recover from.
There is a small possible-mini-seizure story to be told from the weekend, which of course means more appointments for me, and no driving until we figure it out, and continued gooney drugs (anti-seizure prophylaxis) way longer than planned, which is unfortunate because I don’t like feeling drunk and a bit unstable on my feet. And also I can’t drive if I’m going to be at risk for seizures. But it might have just been dehydration, or–my hypothesis–a 90-second seizure secondary to brain disturbance from the SRS plus dehydration/heat/electrolyte imbalance, not to be repeated because it was due to treatment & post-treatment effects, which are temporary! Meanwhile I have other things to follow up on this month–the DVT, the knee pain, my usual 3-month CT scan–which felt a bit overwhelming even before the need for a neurological consult…
In other news, I got approved for disability payments from Social Security in what seems like record time (possibly related to all the records I sent them as instructed…) so at least now my feeling of having too much medical “work” to do is matched by the government’s agreement that I can’t do regular work! I am disabled by my appointments more than by my disease at this point. Who knew?
And now “spa time” in the infusion room is over and it’s off to the coop. Soon I’ll post some pictures from last week’s SRS adventure.
This afternoon is the first of my brain zaps for very small tumors. The radiation oncologist wants to do them one at a time over three days, so we will be at Albany Med Tuesday through Friday, every afternoon. Argh! It’s like a job…but with mind-altering drugs (Ativan, Keppra).