It’s my chemo-versary today: one year ago today I started chemo. So here I am, no sicker. Which is apparently a major triumph “in the metastatic breast cancer setting.” Because even knowing that the statistics are about 5 years behind current treatment options, and even knowing that statistics don’t really apply to any one individual, the MBC survival curve seems dauntingly grim: the studies and articles I am reading all say things like “a median survival from the time of developing metastases rarely exceeding one year.”
So here I am in month 14, celebrating a year of effective chemotherapy. I think I’m on cycle 17. Go, Eribulin. Go, me.
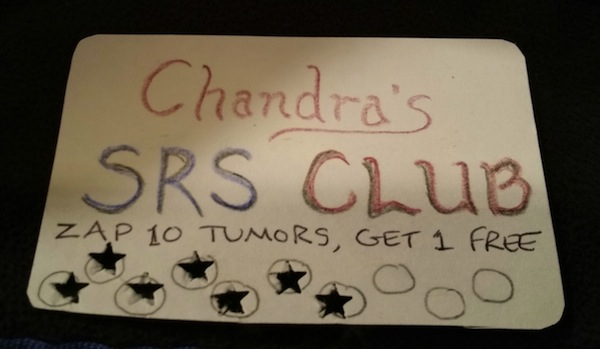
Yes, I have brain mets again…small wrinkle in the plan, it must be admitted. The schedule is to zap them with SRS on Thursday, coincidentally one year to the day after my first zapping procedure. There are only two mets this time and they are smaller than a year ago and both are in easy-to-target spots, so I assume the procedure will be lots quicker and easier. Then a week after that, back to chemo again. This chemo doesn’t cross the blood-brain barrier (as far as researchers know so far) so having new brain mets doesn’t mean it’s not working everywhere it reaches.
The two metastases that chemo does reach are holding steady–not growing, not shrinking. I wish I could see them. Why is there no fancy 4-D ultrasound for anything but in-utero babies? I could use a good visual. There might be a tiny second bone met in one lower-back vertebra or it could be some other little blip seen via the miracle of MRI–so I’m not worrying about that. And most important: no new metastases in any organs. These mets I’m apparently stuck with for now are not affecting me. Very well behaved.
For an extensive review of how things are, triggered by the chemo-versary thing, keep reading below these great pictures!

And here are pictures of a couple other important people!

- Will on Christmas Day

- Jesse on Christmas Day
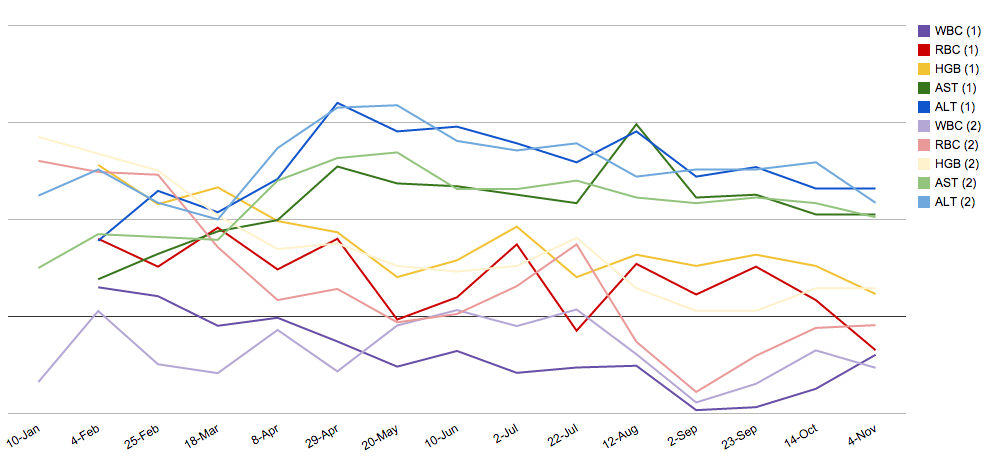
Though I am technically a tiny bit anemic lately, my red blood cell counts are still reasonable (always so far in the normal range, even if lately lurking at the very bottom dregs of normal); I don't know what they're up to (down to) on my weeks off because I don't get tested then, but I think I can feel my mild anemia sometimes then when exercising. My white blood cells are surviving, too--always "normal" except one week when they were low. I don't think I've gotten sick more often than usual, or had a cold for longer than usual. There is a slow downward drift to these numbers but I'm not near needing to do anything about them. (Anything: delay chemo, get blood-count-increasing shots, get transfusions, stop chemo.)
My hair is curly. Though it is thinning a lot (since November?) and right now looks a little pitiful, I am feeling lucky to have gotten hair back at all after the first few months of chemo (it came out about a month after I started, but grew back as soon as my Eribulin dose was reduced in April). Why it is thinning so much is a mystery. Nothing has changed…is it a cumulative build-up of something toxic in the hair follicles? Or the natural life cycle of hairs, which are all unusually synchronized because they all grew from nothing in early May? Or…? Brain zapping may make patches of it fall out again soon anyway, so we’ll see what will make me feel the least pitiful: shaving it all off (brrr, in winter)? Covering the thinnest parts with a bandanna or a hat? Or just embracing the humbling experience–otherwise unattainable for the 51%–of male-pattern baldness? Um, no, probably not that last option.
Hmm, much of navigating the having of cancer, for me, seems to be about figuring out what will make me feel the least pitiful. (In fact the worst thing about nausea & vomiting caused by chemo–which I don’t have this time around, so far! at all!–is how pitiful it made me feel.) The realm of hair contains, apparently, much potential for pitifulness.
I definitely have fewer eyebrows and eyelashes than I did a year ago. A minimal number of eyelashes, probably so few that mascara would just accentuate the weirdness, and besides I have never liked the feeling of gunk on my lashes. My eyebrows need help because on one side I have an eyebrow that stops halfway along, almost, and on the other, 2/3 of the way along. Luckily I started out long ago with really thick eyebrows, which chemo in 2006 thinned out some, but I still had some to spare a year ago. SRS mask-making accidentally ripped some of them out (like waxing?) and then by summer I had figured out (with help and advice) a “prosthetic eyebrow” technique using a brow pencil and stuff that is basically brow mascara. Is it good luck that the current “eyebrow fashion” is very thin, very fakey eyebrows? Mine, prosthetically enhanced, still look more like mine (messy, thicker).
Oh, there I go about hair again.
I am in better shape that I was a year ago, in some ways, due to interval training, jogging, and some strength training. I’ve done all this with the help and company of various relatives and friends at QIVC–which means we’re all getting healthier, not just me! That’s fun. It also gives some of us a bit of social interaction daily in these cold indoor-oriented winter days. I’m grateful to everyone who has jumped on the exercise bandwagon with me, especially my almost-niece Carolyn, who agreed to be my personal trainer and get me doing all this stuff. (It was my trip to the Block Center in late July that got me started on Lots More Exercise.)
But I also am at maybe 80-90% of my old physical energy and stamina for normal life, it feels like, and am frequently achy and stiff. Plus I keep hurting my shoulders by doing nothing in particular beyond some pushups, and then mysterious things like sciatic pain show up and stay for a few weeks. More importantly, it is harder lately to get my brain to focus in on anything complicated. I am very distractible. Chemo brain? Or just lots of distracting aspects of my current life?
I take a lot more supplements now, after a lot of research on each of them. I’ve been getting IV Vitamin C steadily since May, and acupuncture as well. And I eat more kale, broccoli, mushrooms, and salmon. (Here is the best cancer-fighting meal ever: Salmon sashimi, seaweed salad, green tea, and shiitake mushrooms. I guess you could add some grilled broccoli with miso sauce if you had room.)
All summer our garden produced a bounty of kale (enough for us to give lots away, too: we had 50 plants!) and I developed my kale and fruit smoothie: kale, lime juice, a bit of OJ, a bit of kefir (like yogurt), banana, mango, pineapple, flax oil, and glutamine powder. Will & Jesse & Eric like to have some too. I spend a lot more time on my weird foods than I did a year ago–besides the daily smoothie, I also drink a green drink full of broccoli sprout powder etc. (ick) and sometimes make seaweed salad with dulse & Japanese seasoned salt and vinegar. When I travel I have that with breakfast. I am still struggling to avoid meat more often, because I like it so much. The whole family has cut down on dairy products but good cheese is still too hard to resist. We now buy a lot of oat milk, hazelnut milk, and almond milk and I make my own kefir instead of buying yogurt. When I’m stressed and feeling pitiful I still want candy. But mostly I just indulge sometimes in 80% cacao dark chocolate.
So that’s the summary of now vs. January 2014. The coming week is pretty full with appointments and the rest of life, but I will plan to post something after my brain has been zapped again and I have thus developed a new superpower. Wonder what it will be? Nominations welcome.
 Eric has fun drawing on a picture of me with his phone
Eric has fun drawing on a picture of me with his phone