Some, less, and more
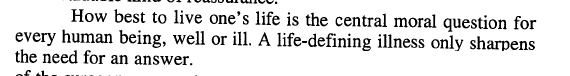
This week I started my fifth round of eribulin. I am very tired of wearing head coverings all day. My radiation “crop circles” have not grown back. Maybe they won’t. Or maybe it will take six months. The oracle of the Internet (accounts of other metastatic breast cancer people) is not clear on the subject.
Some: late last week (my week “off” chemo) I started feeling some numbness in my right hand. Then my left hand. Then early this week my right foot, and my shins, and my left foot. It is all superficial–only light touch feels funny. The nerves below the epidermis are working, but the most superficial nerves are damaged. This is a common (50%?) side effect of my and many other chemotherapies: peripheral neuropathy, which can be numbness, tingling, pain, or cold- or heat-sensitivity, or a combination. A little superficial numbness is not too bad. It is not affecting what I can do, or my balance, or anything. It just feels Really Weird.
**Less: **Because of the neuropathy, we reduced the dose of my chemo as of this week. There is a standard dose reduction that is apparently needed for many people who take this drug for a while. It still works with the reduced dose. Of course I asked about the big EMBRACE trial that showed how good this drug is: if 30% or more of the people who took the drug in the trial ended up on a reduced dose, did they look at those patients’ outcomes in comparison to the full-dose patients’ outcomes? You’d think they would have. But I think in real life the course of care and doses of chemo given to patients in the trial were not clearly sub-settable. People switched to the lower dose at different times. People skipped doses or delayed doses due to low white or red blood cell counts (which hasn’t been at all a problem for me). I bet sometime in the future, though, as eribulin becomes used earlier in the metastatic disease process (most people don’t get to try it first like me), there will be a trial of the reduced dose vs. the full dose to see if the reduced dose is just as good. Until then, people who can’t handle the full dose anymore get the reduced dose, and it works as well as it works. My oncologist’s take on it seems to be: as long as it works for some people, it’s worth trying in any one person, so who needs the data from the subgroup? The subgroup analysis won’t tell him whether the lower dose will work for me or not. I guess that makes sense. But if the lower dose didn’t work for anyone, wouldn’t that be important to find out as part of the trial?
I’m also trying to eat less dairy. Very sad.
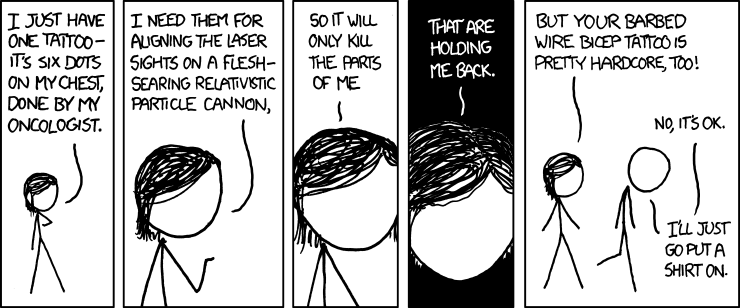
**More: **To start with the simple, I am drinking at least one cup of very-well-steeped green tea every day. Moving on abruptly to the incredibly complex, I now have more healthcare providers. Last week I began going to the Stram Center for Integrative Medicine in Delmar (next to Albany) because I want to get IV Vitamin C (which they offer) and because I want guidance on nutrition and supplements. I will also most likely try their acupuncture person and see if acupuncture feels more beneficial for me than it did in 2006. My initial meeting involved a health history and the creation of a long list of blood tests that will guide their recommendations. They’re all about inflammation, immune system function, coagulation, vitamin and mineral levels, etc. My oncologist agreed to run a few of these and yesterday my primary-care doctor spent a totally un-American amount of his afternoon with me, working through the remainder of the tests, reviewing the logic of them per Dr. Stram and other sources, and figuring out exactly which ones to order. Now I can just go to the lab and give them a pint of blood, right? Wrong. More homework: I need clarification from the Stram Center about 3 or 4 tests that we couldn’t pin down yesterday. I need to talk to my health-insurance company about what happens when they refuse to cover many of these (they are oddball): do I pay the lab’s list price or the “reasonable and customary” price that the health-insurance company would have paid? And then I need to talk to the lab and get the prices for these tests, because if some of them are hundreds of dollars, I most likely need more discussion of their utility with Dr. Stram before I do them.
Less: calling people “doctor.” He said they use first names so he is Ron.
Less: time to do paying work and schoolwork in the last week…but also, less fatigue on my last week “off” than the cycle before, and the last few days, less queasiness (none so far!) and less feeling generally under the weather and kind of poisoned. Still not feeling great, but not in bed, and it’s only been two days since chemo.
More: At the Stram Center I also met with a nutritionist/dietician with a certification in oncology nutrition. (He comes from the Block Center in Skokie, IL where I would be going if I lived nearer. It is an integrative oncology clinic.) It would be such a luxury to have one set of providers rather than trying to cobble things together…but the reason for the Stram Center is to avoid extreme cobbling. There is my offensive team (oncologist and oncology nurses) and now my defensive team: the integrative practice. (See the link on the right for more info about their cancer services.) The goal of going there–what “defense” means to me right now–is to try to adjust anything in my body that can be adjusted to be less favorable to tumor growth & spread. The lab tests, according to them, will guide them in suggesting adjustments. And also to try to minimize side effects–they have suggestions for fatigue, queasiness, and neuropathy. The IV Vitamin C helps with side effects too. Looks like I have a lot of work to do before I get there, though.